Send Us A Message
View Our Newsletter
Schedule A Demo
FAQs
We Are National
The Compliance Store is the only comprehensive online regulatory resource designed for long-term care. It provides anytime access to updated regulatory and government agency information.

About Us
The Compliance Store is the only comprehensive online regulatory resource designed for long-term care. It provides anytime access to updated regulatory and government agency information.

Our Solutions
Thousands of crucial documents at a moment’s notice. Manuals and other information continually updated in real-time. Including the only compendium of state regulations available anywhere.

Your Subscription
Your subscription to The Compliance Store includes access to all of the information and resources on our website.Clinical
To help meet your compliance requirements, we have Tools & Templates to help you manage and educate your staff, respond to deficiencies in a timely manner and maintain compliance.
MDS
MDS/Care Plan Coordinators and Nurse Managers will have access to REAL-TIME MDS and regulatory updates and revisions, including the latest changes in reimbursement.
Administrative
Your bottom line is important in a constantly changing regulatory environment. Facility Administration and Corporate Management will stay informed of money management information to maximize the bottom line.
Interdisciplinary Team
Our fully-optimized search engine gives your healthcare IDT instant access to information important to the safety of your residents and employees. We have comprehensive information relevant to your bottom line.
Survey
Administrators, Directors of Nursing, and your entire team have plenty to do every day without having to worry when surveyors show up. We will have you prepared with all the regulatory and compliance information needed.
More than 50 Years of Experience in Long-Term Care
Satisfaction
Subscribers
regulatory websites
updates last year

Bill Turenne
Owner & CEO

Janet Eastwood
Owner

Craig Biser
Executive Vice President

Phil Hayes
Executive Vice President

Emily Walls
Chief Financial Officer

Jeremy Alphord
Vice President, Marketing & Communications

Josh Stuedeman
General Manager

Michele Mummert
Research & Development Director

Donna Adendorff
Research & Development Consultant

Jaime Butler
National Sales Manager

Brandon Stephens
National Sales Representative

Lorrel Filliater
Account Manager

Lee-Ann Arner
Research & Development Coordinator

Emily Foreman
Account Manager

Polly Smith
Content & Development Coordinator

Traci Varon
Operations Coordinator

Marx Misigah
Information Technology Director

Cushing Phillips
WEB & PRODUCT INFORMATION MANAGER

Lauren Wright
Human Resources Director
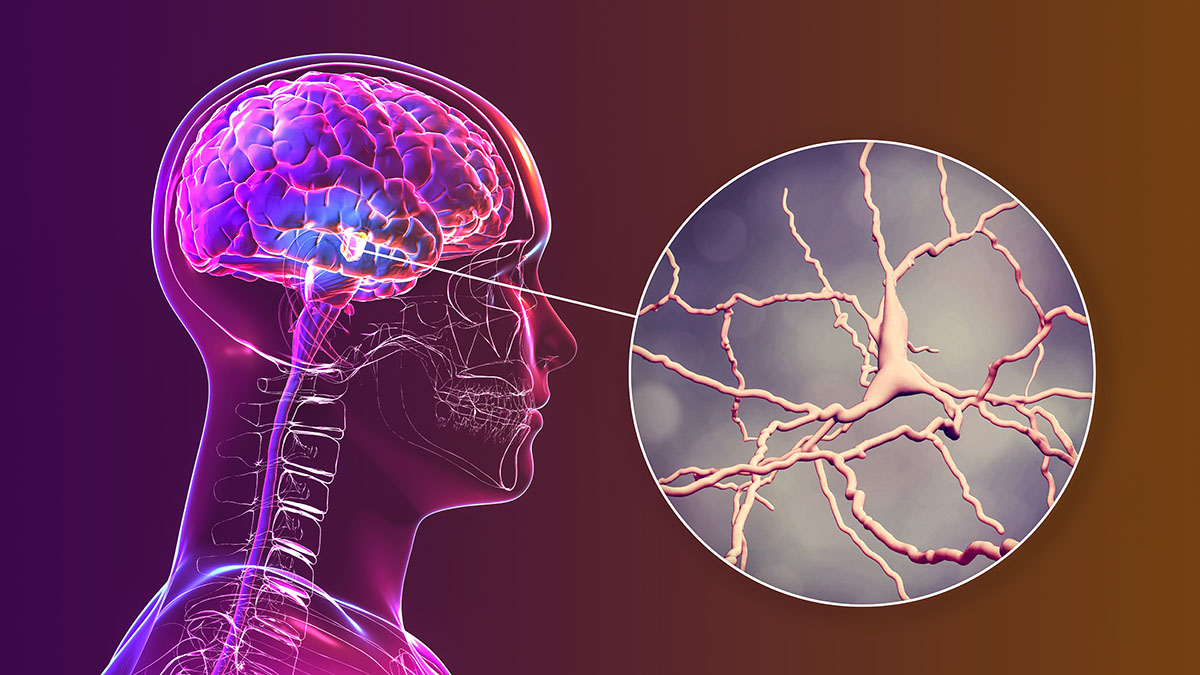
Stroke rehabilitation is vital to helping residents achieve better quality of life
The Compliance Store joins the nation in recognizing this serious condition and the importance of stroke rehabilitation and the part it plays in helping residents...
We are grateful for nurses this Nurses Week
Thank you for enriching the lives of your residents, their families and your communities. We wish you a great National Nurses Week!
14 warning signs of Parkinson’s disease you need to know
Despite its prevalence, there is still much we don’t understand about the condition and those who suffer from it. This lack of knowledge can lead...
How to overcome ICD-10-CM coding hurdles: a live workshop
The latest ICD-10-CM coding manual has many nuances and is regularly updated. Thus, accurate coding requires an understanding of how to utilize the ICD-10-CM coding...
How to avoid colorectal cancer for older adults
To help you educate your residents and staff about colorectal cancer and other health topics and medical conditions, The Compliance Store has a wealth of...
Social workers help residents and families overcome challenges
Long-term care social workers help residents overcome concerns or challenges by collaboration with staff and clinicians to ensure optimal quality of life.
- There are no upcoming events.
- There are no upcoming events.
Latest Past Events
Skilled Nursing News Clinical Executive Conference
Tampa Marriott Water Street 505 Water Street, TampaWisconsin Directors of Nursing Council Symposium
Fox Cities Exhibition Center 355 W Lawrence Street, AppletonKentucky Association of Health Care Facilities Annual Meeting & Expo
The Galt House Hotel 140 Fourth Street, LouisvilleStop in and see Lorrel as she supports our valuable Kentucky customers. Let her show you all the latest tools available through your membership in The Compliance Store!